Compassionnate eating disorder therapY in San Diego & virtually in California, Washington, Maryland & Utah.
Overview
Eating disorders are complex, multifaceted conditions that impact the mind, body, spirit and our relationships with others. Eating disorders are often rooted in deep emotional pain, trauma and/or systemic pressures. Food and body image struggles can also be a part of one’s neurodiversity.
There is not one singular “cause” for an eating disorder; but the impact on one’s life becomes all-consuming. At Eating Disorder and OCD Therapy, we offer compassionate, evidence based and client-centered treatment to help you heal from disordered eating and reclaim your true sense of self. Whether you’re seeking a San Diego eating disorder therapist for in-person sessions or virtual eating disorder therapy in California, Washington, Utah or Maryland, our mission is to provide you with affirming and deeply meaningful treatment.
UNDERSTANDING EATING DISORDERS
Eating disorders are life-threatening mental health conditions with serious medical complications when left untreated. They impact not only the person but also their families, friends, and partners. Often times eating disorders are like the canary in the coal mine- they signal deeper pain or familial dysfunction. Contrary to popular belief, eating disorders are not about vanity. They develop from a combination of psychological, genetic, environmental, socio-political, and interpersonal factors. Common behaviors associated with eating disorders include:
RESTRICTING:
Restricting food can look like: limiting food intake to control weight or body shape. This can include calorie counting, macro counting, limiting and/or avoiding certain food groups. It is common to start feeling anxious, guilty or shameful when breaking restrictive “food rules”. Often, people restricting themselves are still eating something which can make it hard for people on the outside to detect. Rarely does someone with an eating disorder eat absolutely nothing. These behaviors often serve the purpose not only of changing body size, but also to numb out from difficult emotions and communicate unmet needs. People of all shapes and sizes can have restrictive eating disorders such as Anorexia Nervosa. Not all bodies drastically change and become “underweight” with restriction. Those with higher weight anorexia (also called atypical anorexia) can experience the same medical consequences that someone in a smaller body can. We take this very seriously and utilize a health at every size perspective when working with any eating disorder, at any body size.
PURGING:
Purging is any use of compensatory behaviors after eating such as vomiting, excessive exercise, or misuse of laxatives. These behaviors are often not a one time thing, the cycle can feel addicting, compulsive and hard to untangle from. To classify as bulimia nervosa, must happen at least three times a week for a few months. That being said, purging (specifically self induced vomiting) is one of the most dangerous eating disorder behaviors and any amount of purging deserves psychological attention so that we can prevent it from spiraling. You can actually die from cardiac issues with just one purge. Purging typically involves a cycle of thoughts, emotions and behaviors. We utilize a wide variety of treatment options to help you break the cycle of purging and understand the complexity of letting go of this behavior. We believe harm reduction approaches are incredibly valuable and life saving here.
BINGE EATING
Binge eating looks like: consuming large amounts of food in a short period despite nutritional needs otherwise being met, feeling ashamed of food behaviors, often binging in secret, feeling a loss of control around food and eating well beyond fullness to the point of discomfort and pain.
Binge eating often involves some amount of physical or emotional restriction leading up to the binge. Like all eating disorder behaviors, we need to look below the surface to determine the appropriate interventions for treatment. Binge eating disorder is the most common eating disorder, but also the most stigmatized. It is often left out of discussions when society talks about eating disorders. This is due to how pervasive diet culture is- we live in a world that praises restraint and control around food. Binge eating often feels ego-dystonic to the person and fuels shame. Please know we believe anyone struggling with binge eating deserves compassion, attunement, and just as much care as someone struggling with a restrictive eating disorder.
OSFED:
OSFED or ‘Otherwise Specified Feeding and Eating Disorder’ is the most commonly diagnosed form of an eating disorder. It is used when someone does not fit neatly into diagnostic criteria- i.e. they have some of the symptoms, but not all. Or, they have a handful of symptoms in multiple categories of eating disorders. Humans are multifaceted and complex- we don’t often fit perfectly into checklist boxes of diagnostic criteria. And, diagnostic criteria is often exclusionary of inclusive identities. So, it makes sense that the most common eating disorder is actually OSFED.
It is important to know that OSFED does not mean “less severe.” Research shows that OSFED can be just as deadly and have just as many health consequences. It is important to get help as soon as possible and it is just as valid. Don’t let anyone tell you that you aren’t sick enough because you have OSFED and not Anorexia.
ARFID:
Avoidant/Restrictive Food Intake Disorder (ARFID) is an eating disorder characterized by food avoidance or restriction that leads to nutritional deficiencies, malnourishment, or difficulty meeting daily energy needs. While body image concerns can absolutely co-occur, it isn’t typically the driving force for the food aversion and is not always present. ARFID is often misunderstood as “picky eating,” but it is far more complex and is often rooted in sensory sensitivities, fear of eating due to a feared consequence such as vomiting, choking or getting sick. ARFID commonly co-occurs with various forms of neurodivergence such as autism or ADHD. Our approach to treating ARFID is neurodiversity affirming, meaning we honor the client’s sensory needs and food preferences rather than pathologize them or “fixing” them. We focus on creating individualized accommodations that make eating safer, more accessible, and less distressing. While many providers in the eating disorder field believe that treating ARFID means exposure to aversive food and habituating to the distress, we know that this can actually be traumatizing to the client and out of alignment with their goals. Therefore, we aim to get creative with our ARFID clients and look at ways to expand/adapt existing safe foods- and only engage in gradual exposure if that is what the client is wanting.
*It is worth noting that many eating disorder behaviors exist together. We rarely fit neatly into diagnostic categories and your eating disorder is no less valid if it is not perfectly captured by a specific diagnosis
Who is Eating Disorder Therapy For?
We work with adolescents and adults of all genders and identities who are experiencing:
Anorexia- including ‘Atypical’ Anorexia, or any form of restrictive eating
Binge Eating Disorder (BED)
Bulimia Nervosa and purging behaviors
ARFID (Avoidant/Restrictive Food Intake Disorder)
Mixed eating disorder presentations
We specialize in supporting BIPOC, neurodivergent, LGBTQAI+ folks, and those navigating the impacts of trauma, anti-fatness, and other forms of systemic oppression alongside their eating disorder.
While diagnosis can be validating for some people, it isn’t necessary to meet certain criteria to work with us. We firmly believe that any amount of suffering with food and body image warrants support. Early intervention is best when it comes to recovery from an eating disorder- you don’t have to wait for it to get worse.
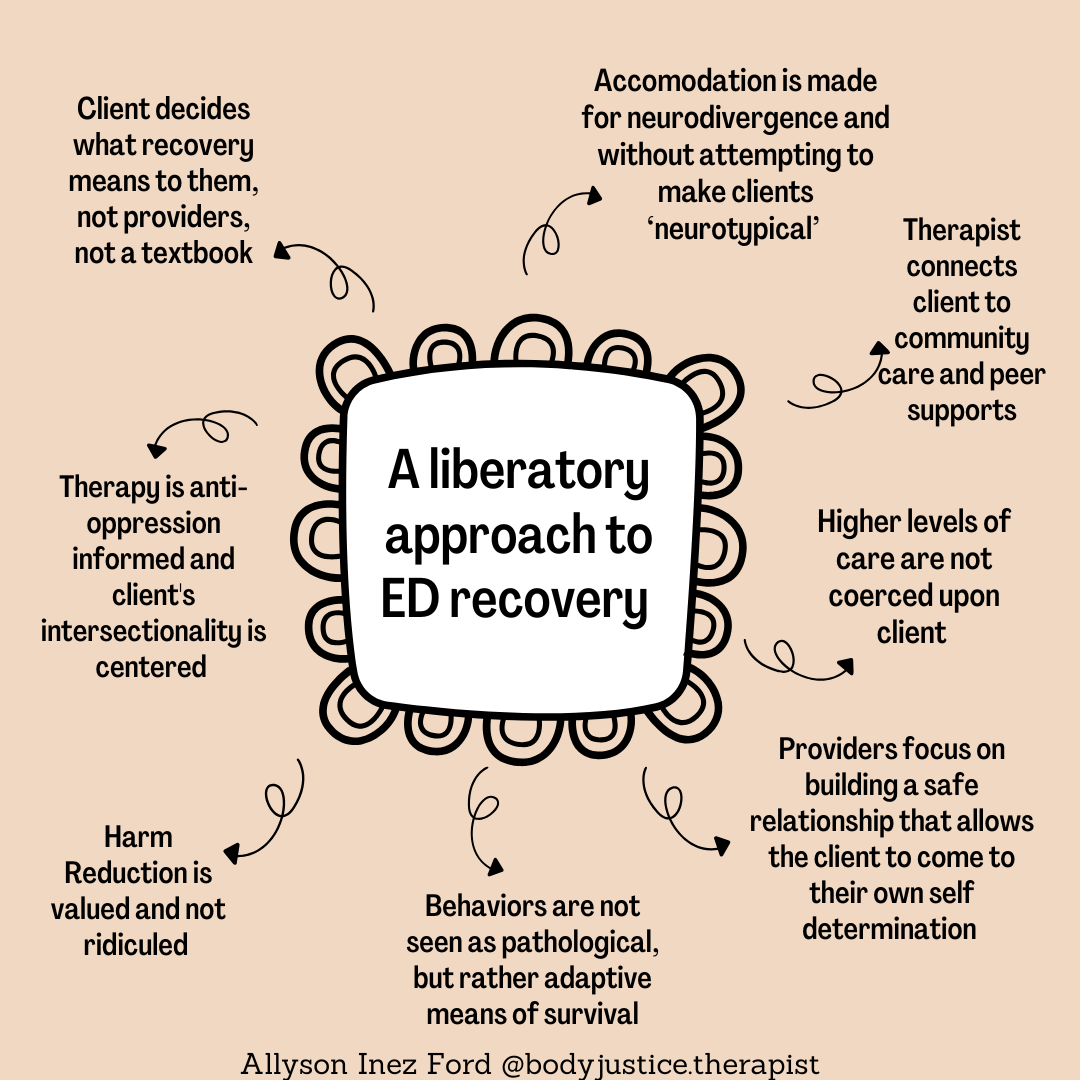
Therapeutic Approach
Our approach is grounded in a relational psychodynamic framework, feminist therapy, neurodiversity affirming care and is trauma-informed. We use components of DBT, CBT, ERP and ACT as well. We see eating disorders not as vanity or choice, but as understandable coping mechanisms developed in response to deep suffering. Treatment is individualized and collaborative- you drive the boat and we are your supportive guide.
Modalities we often use and blend in our work with clients:
Common Client Goals
Stop or reduce restricting, bingeing, purging, or over-exercising
Reconnect with hunger, fullness, and body cues OR learn to eat mechanically according to your body’s unique needs (not everyone can sense body cues- but this doesn’t mean recovery isn’t possible)
Heal from trauma and attachment wounds
Feel less obsessed with food, numbers, or appearance
Feel more at peace with your body- you don’t have to LOVE it in order to have a peaceful acceptance of it.
Learn to nourish yourself without fear or guilt
Have freed up brain space to focus on other aspects of life and self
Improve relationships with family and friends
Session Structure & Treatment TeamS
Sessions are available in-person in San Diego or virtually for clients across California, Washington State, Utah, Maryland and Florida. We typically meet weekly, beginning with an in-depth assessment and collaborative treatment planning. Our process is flexible and attuned to your unique needs, readiness, and values. Eating disorder treatment has the most successful outcomes with a treatment team approach. As therapists, we are one part of that; depending on your specific needs and resources, we will likely recommend meeting with an eating disorder specialized dietician, medical doctor, recovery coach or support group in addition to therapy. This becomes your personal recovery team and ensures all aspects of an eating disorder are being adequately addressed. Eating disorders are complex and it takes a village to recover. We can help you with referrals and we will coordinate care with everyone on your team.
Special Features or Techniques
Neurodivergent-affirming care
(focus on accommodations and underlying sensory needs)
Harm reduction approach
aimed at keeping you safe when you aren’t ready to stop using behaviors.
Relational healing
for clients with attachment trauma.
Socio-political and body justice lens
to explore the impacts of oppression on eating/body image.
Somatic, creative, and values-based interventions
to build safety, alignment and joy.
Treatment team model
to build wraparound support and care.
Ketamine Assisted Therapy
to work through stuck points that won’t ease up with traditional approaches.
Collaborative Process
We believe recovery requires autonomy and safety. We don’t force compliance or a specific treatment lens if it isn’t vibing with you. We build a secure therapeutic relationship that is collaborative, where you can explore what healing means on your terms. Together, we uncover what’s beneath the eating disorder and create pathways that feel empowering, not punitive, surface level or coercive.
Client Experience
Clients often share that they finally feel seen and understood here. Many come in feeling like their struggles aren’t “severe enough” or that they don’t fit the stereotypical mold. At ED & OCD Therapy, we affirm all eating disorder experiences and all bodies. Our clients learn to approach themselves with compassion, deepen emotional insight, and slowly disentangle from harmful food/body narratives, while staying grounded in their values.
Long-Term Benefits
Fewer disordered eating behaviors and rituals
Increased capacity for emotional regulation and distress tolerance
Greater self-trust and reconnection with self
Improved relationships and boundaries
Freedom from obsessive thoughts about food and weight
A more empowered and authentic sense of identity
Lasting healing grounded in your own values, not external expectations
Final Thoughts
Recovery is HARD and it is 100% worth it. If you or your loved one is struggling with an eating disorder, please reach out to us at 619-752-4318 to schedule your free 15-minute consultation.
Together, we can work towards a future free from the constraints of disordered eating and towards a life filled with inner peace, meaning, and deep fulfillment.
Ready to start therapy?
⟡
Ready to start therapy? ⟡
At Eating Disorder OCD Therapy, we offer compassionate, relational, and individualized care, rooted in the belief that healing is not one-size-fits-all. Honoring client autonomy, collaboration, and anti-oppressive, neurodiversity-affirming practices, we walk alongside you as the expert in your own life. We provide therapy for Eating Disorders, OCD, Body Image, Trauma, Maternal Mental Health, and offer Ketamine Assisted Psychotherapy (KAP), Group Therapy (globally), Recovery Coaching (globally), and Clinical Consultation and Supervision for clinicians. We are currently accepting new clients for in-person therapy in San Diego and virtual services in California, Washington, Utah, Maryland and Florida.